Thrombin generation profiling in rare coagulation factor deficiencies: associations with bleeding severity and potential for screening
Rare coagulation factor deficiencies (RCFDs) are inherited bleeding disorders with highly variable clinical phenotypes. Even mild deficiencies can cause significant bleeding, yet routine screening tests such as prothrombin time (PT) and activated partial thromboplastin time (APTT) often fail to detect abnormalities. Moreover, coagulation factor activity assays do not reliably predict bleeding tendency in these patients. This limits their usefulness for diagnosis and risk stratification. Thrombin generation assays provide a global assessment of hemostatic capacity and may therefore offer a more accurate reflection of the bleeding phenotype. This study aimed to evaluate thrombin generation in relation to bleeding severity and to compare its screening performance with PT and APTT in patients with congenital deficiencies of factors II, V, VII, X, XI, and combined FV/FVIII deficiency.
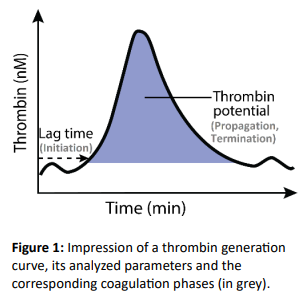
Thrombin generation was measured using the Nijmegen Hemostasis Assay in RCFD patients included in the Rare Bleeding disorders in the Netherlands study (RBiN, 2017-2019). Parameters analyzed included lag time and thrombin potential, reflecting the initiation and propagation/termination phases of coagulation, respectively, and the combined thrombin potential-to-lag time (TP/LT) ratio, providing an overall measure of coagulation efficiency (Figure 1). Lower TP/LT ratios indicate impaired coagulation. Values were normalized using pooled normal plasma and expressed as percentages of the mean from a healthy control cohort. Thrombin generation data were correlated with bleeding severity grades (BSG), and assay sensitivity was compared with APTT and PT.
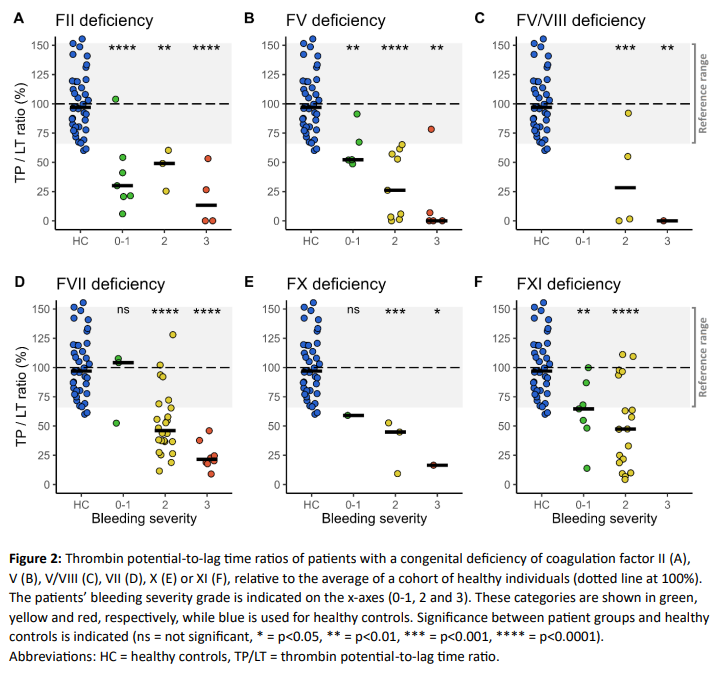
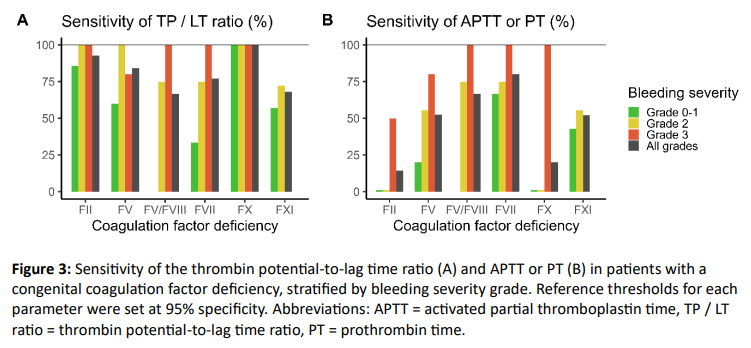
A total of 106 patients with RCFDs (median age 40 years, 53% female) and 37 healthy controls (median age 46 years, 57% female) were included. Most patients had mild to moderate deficiencies (median factor activity 35%, IQR 7-52%). Overall, thrombin generation was significantly reduced in patients compared to controls (Figure 2). Analysis of individual parameters showed that prolonged lag times, particularly in FVII deficiency, and decreased thrombin potentials both contributed to reduced TP/LT ratios that were associated with bleeding severity. Median TP/LT ratios ranged from 30-104% in patients without spontaneous bleeding (BSG 0-1), 26-49% in those with mild spontaneous bleeding (BSG 2), and 0-22% in patients with severe spontaneous bleeding (BSG 3), depending on the specific deficiency. At 95% specificity, the TP/LT ratio showed sensitivities of 68–100%, outperforming APTT and PT (14–80%) in all RCFDs except FVII and combined FV/FVIII deficiency (Figure 3). Particularly in FII and FV deficiencies, conventional assays frequently failed to detect affected patients, whereas the TP/LT ratio maintained high sensitivity.
Thrombin generation profiling correlated with bleeding severity and showed higher sensitivity than conventional screening assays in RCFD patients. These findings support the clinical potential of thrombin generation assays in the screening and clinical evaluation of secondary hemostatic disorders.