The Pulmonary Embolism Rule-out Criteria (PERC) to rule out acute pulmonary embolism in patients with sickle cell disease: a retrospective cohort study
Sickle cell disease (SCD) is a hypercoagulable state and associated with an increased risk of venous thromboembolism (VTE). Patients with SCD frequently present at the emergency department (ED) due to vaso-occlusive painful episodes (VOE). However, these patients are often suspected of acute pulmonary embolism (PE) due to overlapping symptoms, potentially resulting in over-diagnosis with Computed Tomography Pulmonary Angiography (CTPA). Currently, there is no reliable method to safely rule out PE in SCD patients. D-dimer levels are chronically high in SCD, making D-dimer-based criteria like YEARS ineffective. The Pulmonary Embolism Rule-out Criteria (PERC) is used to rule out PE in low-risk patients (<15%), based on clinical gestalt or low Wells score.
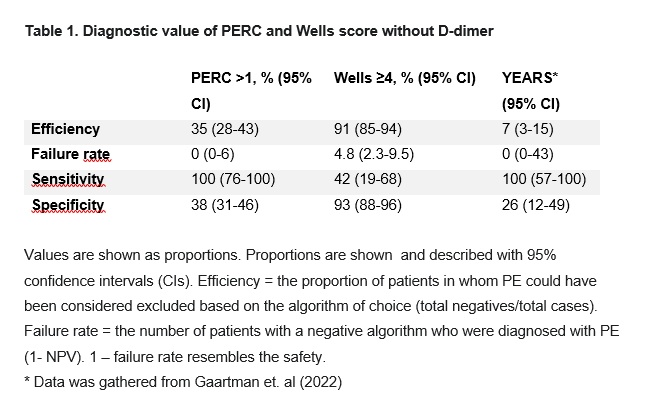
This study retrospectively assessed the diagnostic accuracy of the PERC in SCD patients suspected of PE who had undergone CTPA. This single-center retrospective study analyzed SCD patients who underwent CTPA for suspected PE, using data from electronic records. Sensitivity, specificity, efficiency, and failure rate of the PERC criteria and a Wells score (without D-dimer) were calculated with 95% confidence interval (CI). PE was considered excluded if no PERC were met. We also examined the link between chest pain not recognized as VOE and a PE diagnosis.
A total of 162 CTPAs were performed in 67 SCD patients (median age 34, 61% female). Of these, 119 (72%) were in patients with HbSS/HbSβ0 and 45 (28%) in patients with HbSC/HbSβ+. PE was confirmed in 12 cases (7.3%). As shown in table 1, PERC had 100% sensitivity (95% CI: 76%-100%) and 38% specificity (95% CI: 31%-46%) with an efficiency of 35% (95% CI: 28%-43%) and a failure rate of 0% (95% CI 0%-6%). A Wells score of >4 without D-dimer showed a sensitivity and specificity of 42% (95% CI: 19%-68%) and 93% (95% CI: 88%-96%) respectively, with an efficiency and a failure rate of 91% (95% CI: 80%-91%) and 4.8% (95% CI: 2.3%-9.5%) respectively. Chest pain not identified as VOE was predictive of PE with 83% sensitivity, 74% specificity, and a positive and negative likelihood ratio of 3.2 (95% CI 2.2-4.6) and 0.2 (95% CI 0.1-0.8) respectively.
Based on these findings, CTPA could have been withheld in 35% of SCD patients suspected of PE with the PERC while maintaining a failure rate of 0%. Chest pain not recognized as VOE had a strong predictive value in diagnosing PE in SCD patients and adding it to a potential SCD-specific PERC in a larger prospective study might further improve the performance of the PERC.