Occurrence of venous thromboembolism in HbSC disease and sickle cell anemia and association with thromboinflammation
Sickle cell disease (SCD) is characterized by vaso-occlusion and chronic hemolytic anemia. Hemoglobin SC disease (HbSC, heterozygosity for hemoglobin S (HbS) and HbC), is the second most common form of SCD. Compared to the most prevalent form sickle cell anemia (SCA, i.e. HbSS), HbSC has a clearly distinct phenotype and is considered to have a mild phenotype. Growing evidence suggests a high burden of venous thromboembolism (VTE) in SCD patients. This study aimed to investigate the differences in VTE occurrence between HbSC and SCA and identify potential risk factors.
This study was a single-center retrospective electronic chart review of adult patients with SCD. General demographic information, genotype, location of VTE, and lifetime admissions for most common SCD complications were collected. Laboratory values, both at steady state and during the event, were analysed. From a subset of patients with and without a history of VTE whole blood was obtained to measure soluble transferrin receptor (sTFR), hemopexin, heme oxygenase-1, CD40 Ligand, VEGF were assessed with MSD ELISA in plasma. Plasma cytokines were measured with OLINK technology.
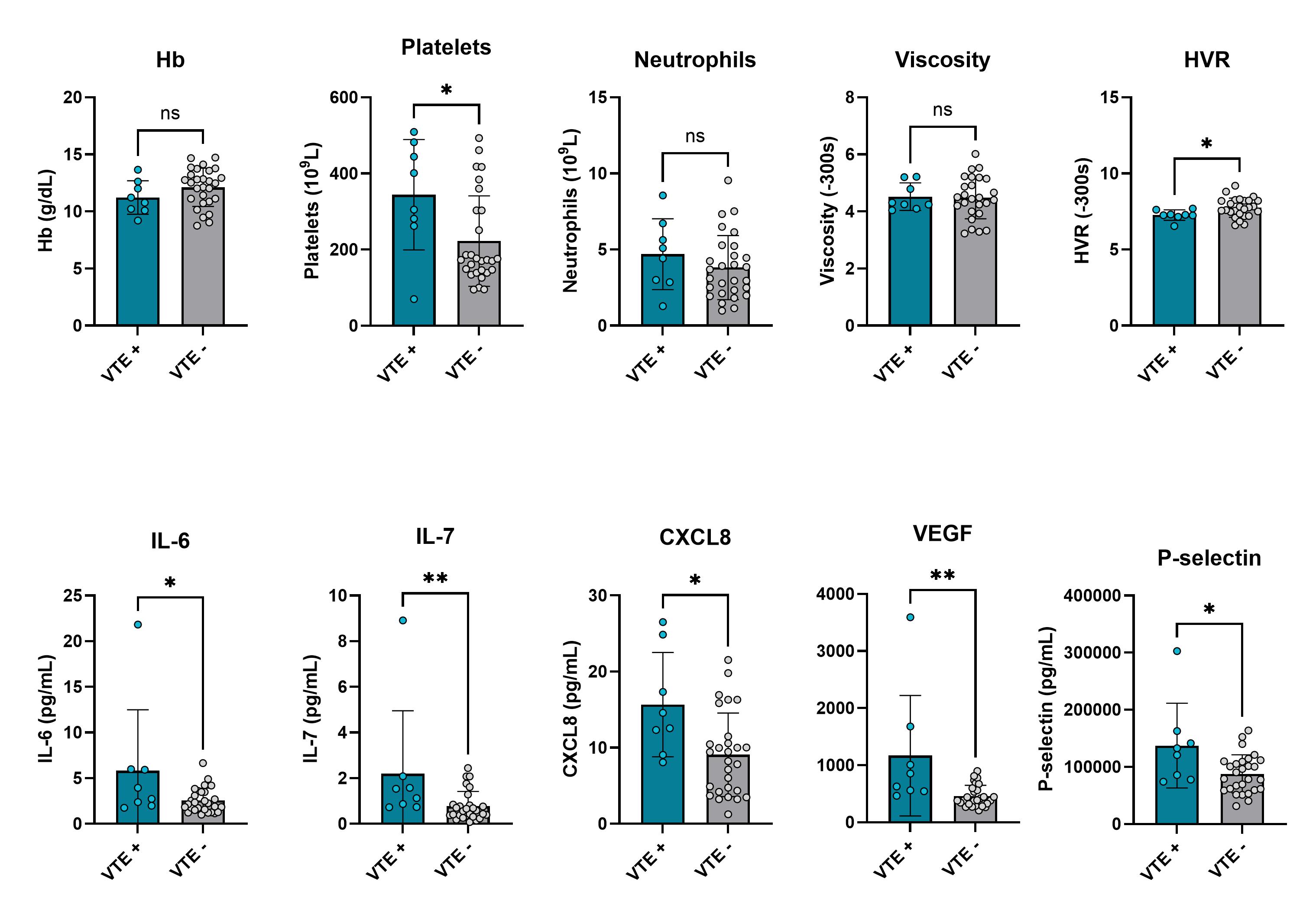
Among 260 individuals with SCD, 22% (58/260) experienced venous thromboembolism (VTE), with no significant difference between genotypes (HbSC 20%, SCA 25%). Pulmonary embolism was the most common type of thrombosis in both HbSC (81%), and SCA (65%). Thrombosis occurred at an older age in HbSC than SCA patients. Recurrent VTE occurred in 28% of cases. Individuals with a history of VTE had a higher leukocyte count, thrombocytes, and lactate dehydrogenase levels (p<0.05). When comparing laboratory values during a thrombotic event with steady state significant lower hemoglobin levels and higher leucocyte count was found in SCA and HbSC patients with a VTE (all P<0.05). In SCA a significant higher lactate dehydrogenase (LD) was found during VTE (p=0.025). We found increased platelets, IL-6, IL-7, CXCL8, VEGF, CDL40, P-selectin and E-selectin in 8 HbSC patients with a history of VTE compared to 26 without VTE (Figure 1). Hemoglobin, hematocrit and viscosity were not significantly different between these 2 groups. In contrast the hematocrit to viscosity ratio (HVR) was lower in HbSC with VTE. When comparing 10 SCA adults with VTE to 42 without VTE, we did not find any significant difference in hematological or thromboinflammatory parameters.
A relatively high burden of VTE was identified, with high prevalence of pulmonary embolisms. Even though prevalence of VTE is comparable between SCA and HbSC, in the latter group VTE is associated with increased inflammatory and adhesion markers. Intriguingly, blood viscosity, hemoglobin or hematocrit levels were not elevated in patients who experienced VTE. Future studies are warranted to further explore differences between HbSC and SCA.