Mapping Treatment Indications and Lines of Therapy in Cold Agglutinin Disease/Syndrome: Insights from Clinical Practice at an Expertise Center
Cold agglutinin-mediated hemolytic anemia (cAIHA) is a rare disease with a prevalence of 5-20 per million. cAIHA is caused by IgM autoantibodies against red blood cells reacting at cold temperatures, resulting in hemolytic anemia through complement activation and acrocyanosis (cold-induced peripheral symptoms; CIPS) through agglutination. cAIHA is categorized into cold agglutinin disease (CAD), in which cold antibodies (CA) exist in absence of an underlying disorder but with presence of B-cell clonality, and cold agglutinin syndrome (CAS), associated with underlying conditions, such as overt lymphomas. While various therapies are under investigation, there is no consensus on an optimal treatment algorithm for cAIHA. More insight into real-world treatment pathways could improve our knowledge of current practice and identify therapeutic challenges for cAIHA patients.
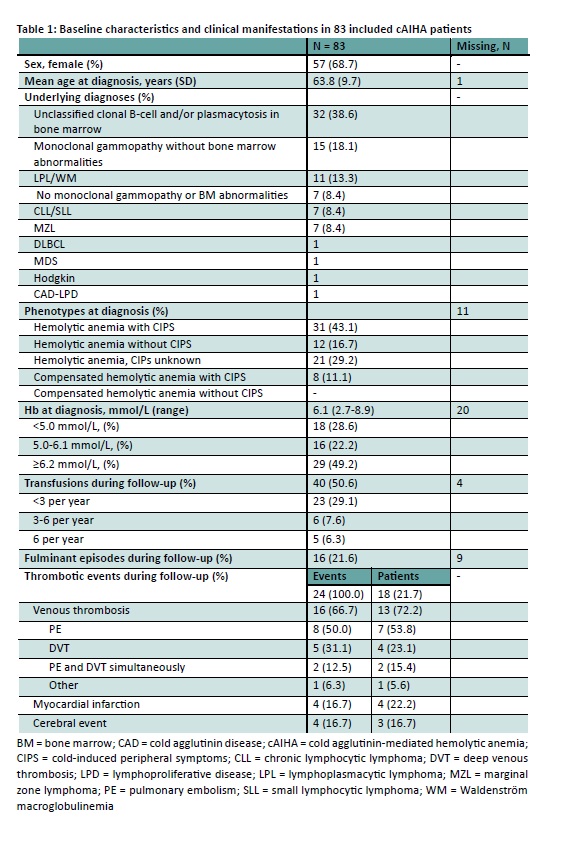
Patients with a cAIHA diagnosis who were seen at our tertiary referral hospital between 2000 and 2025 were included if they had chronic hemolysis, a DAT positive for C3d, and presence of CA. Patients with CAS associated with infections or autoimmune diseases, or who had not undergone a bone marrow biopsy were excluded. Clinical data on diagnosis, disease phenotype, treatment lines, thrombotic events, fulminant episodes (defined as Hb ≤5.0 mmol/L requiring >1 transfusion within 7 days), and transfusions were collected retrospectively.
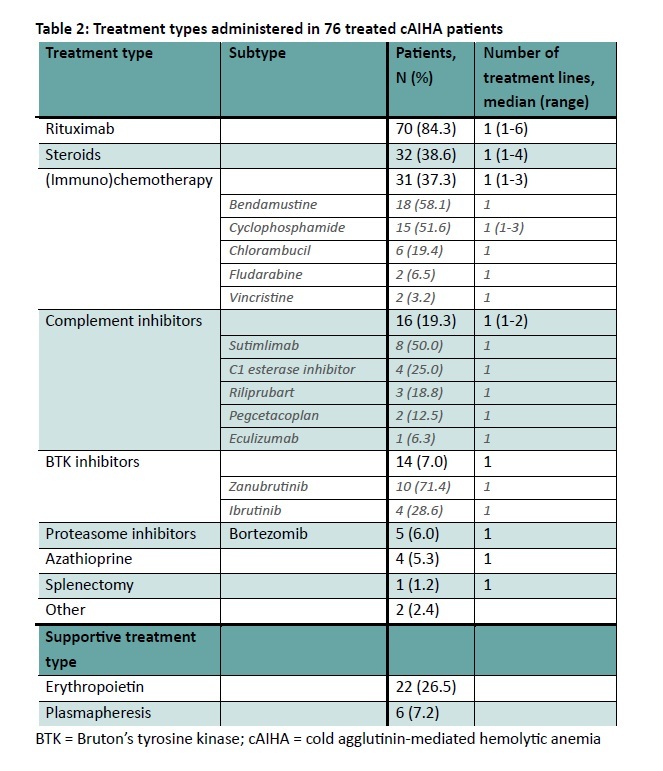
Eighty-three patients were included. Mean age at diagnosis was 63.8 (SD 9.7) and 57 patients (69%) were female (Table 1). At diagnosis, median hemoglobin level was 6.1 mmol/L (range 2.7-8.9), and 64/72 patients (89%) were anemic. 39/51 patients (76%) presented with CIPS. In 27 patients (32.5%), an evident underlying lymphoma was found. Median follow-up time from diagnosis to last contact was 5.5 years (0-28). During follow-up, 40 patients (48%) received ≥1 blood transfusions, and 16/76 patients (21%) experienced ≥1 fulminant episodes. Twenty-four thrombotic events occurred in 18 patients (22%). Seventy-six patients (92%) received treatment, with a median number of 2 treatment lines (1-12), excluding erythropoietin and plasmapheresis (Table 2). Rituximab was administered to 68/76 patients (84%), with a median of 1 line (1-6). Thirty-two patients (39%) were treated with steroids, and 31 (37%) with (immuno)chemotherapy. During follow-up, 11 patients (13%) died, of which two were possibly cAIHA-related.
This study presents the first insights into treatment pathways in a large cohort of Dutch cAIHA patients. Patients present with a high and varied disease burden, shown by their disease phenotype, frequent occurrence of fulminant episodes, transfusion dependence, and thrombotic events. Most patients require treatment, often more than once, with a wide range of regimens being administered. These results highlight the need for improved knowledge on treatment choices and the development of more effective therapies, potentially tailored to disease phenotype.